Editorial for WIROC 22 Issue
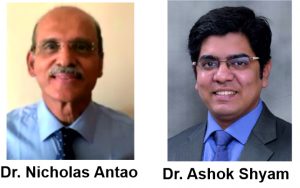
Journal of Clinical Orthopaedics | Vol 7 | Issue 1 | Jan-Jun 2022 | page: 1 | Dr. Nicholas Antao, Dr. Ashok Shyam
DOI: 10.13107/jcorth.2022.v07i01.453
Author: Dr. Nicholas Antao [1], Dr. Ashok Shyam [2]
[1] Department of Orthopaedics, Hill Way Clinic, Hill N Dale Building, 4th Floor, Hill Road, Bandra West, Mumbai, Maharashtra, India
[2] Department of Orthopaedics, Sancheti Institute for Orthopaedics and Rehablitation, Pune, India
Address of Correspondence
Dr. Nicholas Antao
Head of Department of Orthopaedics, Holy Spirit Hospital, Mahakali Road, Andheri (E), Mumbai – 400093, Maharashtra, India.
Email: narantao@gmail.com
Editorial for WIROC 22 Issue
The 2019 WIROC issue featured the first symposium on surgical site infections, spearheaded by Dr. Gautam Zaveri. Our symposium in the 2022 WIROC issue, the brainchild of Dr. Vishall Kundnani and team, features a special on spine pathology. It has contributions from stalwarts of spinal surgery all over India in the form of case reports, review articles, original articles, imaging and diagnostic tests, meta-analysis, arthroscopy-assisted spinal surgery, and current trends in spinal surgery. It provides insight into the challenges associated with the diagnosis and management of various spinal ailments, which can cause our patients significant distress.
Our four guest editorials include heart-warming messages from Dr. S. Gawhale, Bombay Orthopedic Society President, Dr. Kushall Kundnani, Dr. K. Badani, and Dr. Kshitij Chaudhary. We are fortunate that Dr. Bhaskar Anand, winner of Indian Society of Hand Surgery Award for lifetime achievement, has contributed his rich experience in dealing with CLUB hand. We feature a highly informative review article on management of the 1st time shoulder dislocators as well as an inspiring research article on newer concepts in the 1st time patellar dislocators. An original article summarizing the technique of Arthroscopic Latarjet management of shoulder instability is particular enlightening as it simplifies a difficult surgery in a succinct manner.
The landscape of joint replacement surgery is ever changing with newer techniques of uncemented knee joint replacement receiving positive reviews in meta-analyses. Therefore, we have also featured an article on cementless knee replacement, which is an eye opener to the progress of science and technology. An article on the severity of violence of irate patient relatives toward doctors is frightening, but thought provoking. It guides the reader on how to take various preventive measures when faced with aggression and violence. The role of ultrasonography of the hip reveals how hip pathologies can be identified in their infancy, especially in the neonatal setting. Finally, a potpourri of articles in trauma of the foot and ankle is both stimulating and informative.
I am certain our readers will be enriched by the information discussed in this issue and utilize the knowledge gained to provide the
best evidence-based care to their patients.
Dr. Nicholas Antao.
Dr. Ashok Shyam.
| How to Cite this article: Antao N, Shyam AK. Editorial for WIROC 22 Issue. Journal of Clinical Orthopaedics Jan-Jun 2022;7(1):1. |
(Abstract Full Text HTML) (Download PDF)